January was quite a month. With everything happening around COVID-19 vaccines and events in Washington, some big news in healthcare managed to stay out of the headlines.
If you follow drug prices in this country, however, two stories were attention-grabbers. Both underscored the importance and power of transparency.
Senate Sheds Light on Insulin Pricing Practices
Remember when pharmaceutical manufacturers and pharmacy benefit managers were called to testify before the Senate Finance Committee in 2019?
In those live hearings, no one had to divulge much while the C-SPAN cameras were rolling. But the insulin manufacturers in the group did have to submit some 100,000 pages of internal company documents as part of a Senate investigation into pricing practices. Among the findings from the 2-year study, published on Jan. 14:
- List prices for the companies’ top insulin products rose an average of 58 percent in just 5 years (2013-18 or 2014-19, depending on the company’s data provided).
- Contracting practices by intermediaries have done little to discourage higher list prices.
- Rebate amounts for insulins have increased exponentially since 2013.
- Medicare and its beneficiaries spent increasingly more on insulin despite the higher rebate amounts.
- Insulin R&D spending was a small fraction of manufacturers’ revenue and sales and marketing expenses.
The 90-page report pulls back the curtain on pharma business terms, rebates, administrative fees and other details that have never been available to the public before. It also brings into focus the list-rebate-net pricing dynamic and its consequences for diabetes patients.
I don’t know which is more unbelievable—the revelations in this public report, or that more reporters haven’t brought them to the public’s attention.
Hospital Transparency Rule Delivers Right Away
In December, our CEO Michael Rea wrote about proposed rules that, if finalized, could have real impact starting as soon as this year. The Hospital Price Transparency rule (CMS-1717-F2) went into effect in January, requiring hospitals to publish payer-negotiated rates for items and services they provide, including hospital-administered drugs.
Audits after the first month revealed some astonishing early takeaways:
- Health plans (just like consumers) can be charged dramatically different prices for the exact same drugs.
- Hospitals mark up the average sales price of some drugs by an average of 250%.
- Hospitals can actually bank more profit from these drugs than the manufacturers do.
Check out the data in this chart, courtesy of Ronny Gal at Sanford C. Bernstein & Co., showing the prices paid by third-party payers to a sample of five different hospitals for five common drugs:
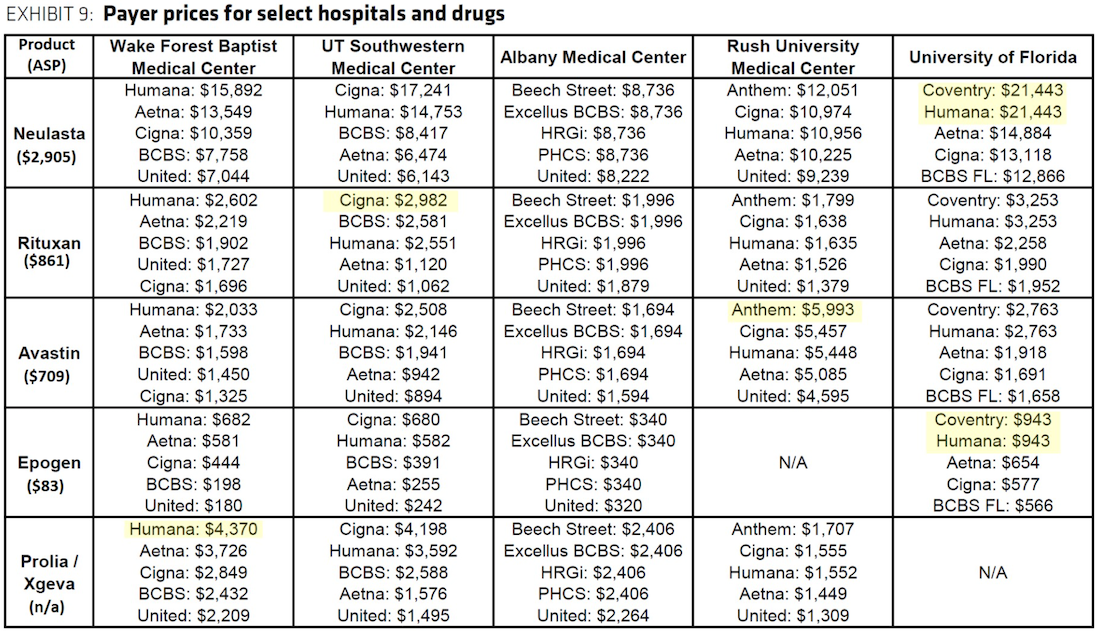 (Drug prices that select hospitals negotiated with third-party payers and reported to CMS. Highlight marks are the chart creator’s.)
(Drug prices that select hospitals negotiated with third-party payers and reported to CMS. Highlight marks are the chart creator’s.)
Granted, the analysis we’ve seen is limited to a small number of hospitals that complied with the rule on time. I’m sure much more insight is forthcoming as more hospitals comply.
Turning the Corner
Shocking as the discoveries may be, we should all be encouraged by these two examples of transparency in action. They are huge steps in the right direction, and by and large are the result of bipartisan efforts at the federal level.
Additional transparency-related rules are on the way in 2022 and beyond, and they promise to create a more educated and sophisticated market that can push down healthcare costs without excessive regulation or legislated reform.
———————————————————-
STAY UP TO DATE
Sign up for our monthly newsletter, The Script, and we’ll send you a quick run-down of industry updates, thought leadership and our latest insightful blogs to keep you informed.

