In preparation for big changes coming to the Medicare prescription drug landscape next year, Part D plan sponsors are working tirelessly to shore-up their budgets and brace for economic and operational impact.
“Margin over membership” is the new resounding approach to weathering a storm of financial pressures brought on by key regulatory, legislative and market developments.
We are seeing this mantra play out in scaled-back supplemental benefit offerings, narrowed provider networks, higher deductibles and market exits. An Oliver Wyman consultant told CNN that this is “the most benefit disruption we’ve seen in the market” in recent years.
Medicare payers are more focused on stability over innovation, consumed by efforts to recover margins and keep an eye on the purse strings. However, the Medicare Advantage Star Ratings program, including the latest changes and adjustments, will require plan sponsors to keep their eye on the ball when it comes to creative thinking and pioneering progress.
Perhaps smart, selective innovation in the name of improving patient outcomes and Star performance holds the key to long-term financial stability.
A Path to Sustainability Written in the STARS?
Over the years, the Star Ratings program has consistently offered plan sponsors a roadmap for improvement – one that ultimately invites innovative approaches to enhancing whole-patient care, outcomes, and satisfaction. It has also served as an additional financial stability lever for plans.
While it may look just a bit different, next year’s roadmap continues to provide opportunities for Medicare Advantage payers to invest in innovation and deliver on quality patient measures. Such investments may even prove to be integral to maintaining long-term economic viability amid new financial pressures bearing down from all angles.
Starting January 1, 2025, CMS will implement key changes to the current program that will impact 2026 Star Ratings – notably, higher cut points across several measures and the removal of contract performance outliers, making high Star Ratings more difficult to come by. Additionally, three brand new patient safety measures will focus on:
- concurrent use of opioids and benzodiazepines
- polypharmacy risks in older adults taking multiple anticholinergic or central nervous system active medications
- kidney health for patients with diabetes
CMS will also make weight increase adjustments to measures focused on improving and maintaining physical health and mental health, along with weight decrease adjustments to patient experience/complaints and access measures (downsizing from 4x to 2x). Furthermore, a new health equity index (HEI) takes effect in 2027 (based on 2024 and 2025 data). Plans will be rewarded for improving care in populations with social risk factors (e.g., low-income, disabled populations).
These changes are intended to inspire creative approaches to meeting patients’ diverse needs and place a stronger emphasis on clinical outcomes and health equity.
Economic consequences for payer non-compliance with quality measures are nothing new. Yet, payers may now consider Star performance a potential budgetary lifeline amid current regulatory and market-level headwinds. Not only from a bonus payment perspective but also in terms of what a heightened focus on patient-centered care could mean for long-term plan viability and profitability.
Clinical Outcomes, Patient-centered Care and Health Equity Reign in 2025. Pharmacy Price Transparency Can Help.
With increased emphasis on achieving better clinical outcomes through patient-centered, high-quality equitable care going into 2025, plans will want to take a harder look at those Star measures (new and old) that are aligned to these goals. Medication adherence can be a critical focal point here with respect to specific age-old measures within the Star Ratings program (diabetes, cholesterol and hypertension) and the broader clinical outcomes landscape in general.
A patient’s medication cost share has long been a key factor in adherence rate. As such, plans may wish to hone their approach to pharmacy price transparency and member decision support as means to drive adherence, boost Star performance, improve overall outcomes and rein in total cost of care through smarter, cost-saving consumer behavior.
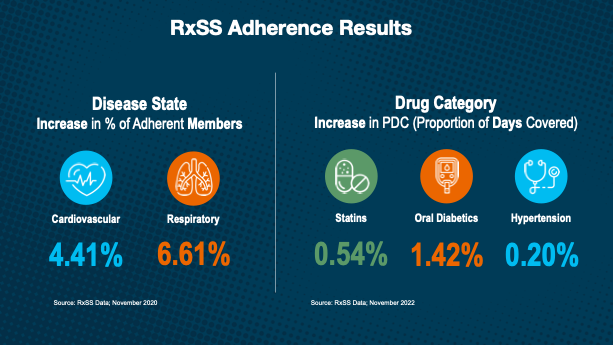
When using a drug price transparency and consumer empowerment tool like Rx Savings Solutions to convert to lower-cost options, Medicare beneficiaries show improvements in proportion of days covered (PDC), reductions in adherence gaps, and increases in recurring refill frequency. All speak to the impact of lower out-of-pocket prescription costs.
Improving Medicare Star Ratings with Pharmacy Transparency
Although member experience Star measures will soon carry less weight, they still make up an important share of a plan’s aggregate Star score and therefore remain critical. Cost-saving, adherent and healthier patients typically are happier, more satisfied patients.
Furthermore, under the new health equity index, pharmacy price transparency can also be leveraged as a vehicle for addressing medication cost and accessibility barriers. Medicare payers have the opportunity to better serve beneficiaries with social risk factors and improve Star performance in this critical area.
The latest Star Ratings’ changes ultimately continue to build upon the Medicare payer roadmap for enhanced patient-centered and equitable health care outcomes. Along with inviting new thinking and creative innovation, the changes offer plan sponsors a chance to step back and assess their broader approach to Star performance at a time when ratings, on average, continue to decline and when market and regulatory pressures are bearing down unforgivingly. Smart, innovative investments today in areas like prescription drug price transparency may hold the key to improved Star performance but also to long-lasting plan viability.
