We are often asked by employers and benefits consultants about one point benefit solution or another, and whether it can deliver on its promise. Our answer: Consider any point solution with a track record of success. One caveat: First, make sure your members can afford their medications.
The market continues to support and adopt these personalized, tech-driven services that address specific health conditions or help close gaps in the healthcare system. But success with point solutions only goes so far as the pharmacy benefit that underpins them all.
Targeting Costly Conditions
Conditions like heart disease and stroke, diabetes, hypertension and mental health account for 90% of America’s $4.1 trillion in annual healthcare expenditures, according to the latest data from the Centers for Disease Control and Prevention (CDC).
CDC estimates these costs will grow by 5.4% annually through 2025, which doesn’t speak to lost productivity or the sheer number of avoidable hospitalizations and deaths. Clearly, our healthcare system has done a poor job helping and motivating people to manage chronic disease.
Enter these and other point solutions that have gained real traction in recent years:
- Livongo and Virta (diabetes, cardiovascular)
- Hinge and Sword (musculoskeletal)
- Spring and Headspace (mental health)
They typically blend clinical specialist expertise, personalization and digital engagement. Wherever they may take a member on the care journey, a medication regimen almost always comes into play.
Estimates suggest more than 238 million Americans suffer from the chronic conditions above. Many are “comorbid,” the clinical term for suffering from more than one condition. These scenarios burden a patient with not only more doctor appointments, potential procedures or complications, but also the cost of multiple medications to treat the underlying conditions.
The Rx Factor
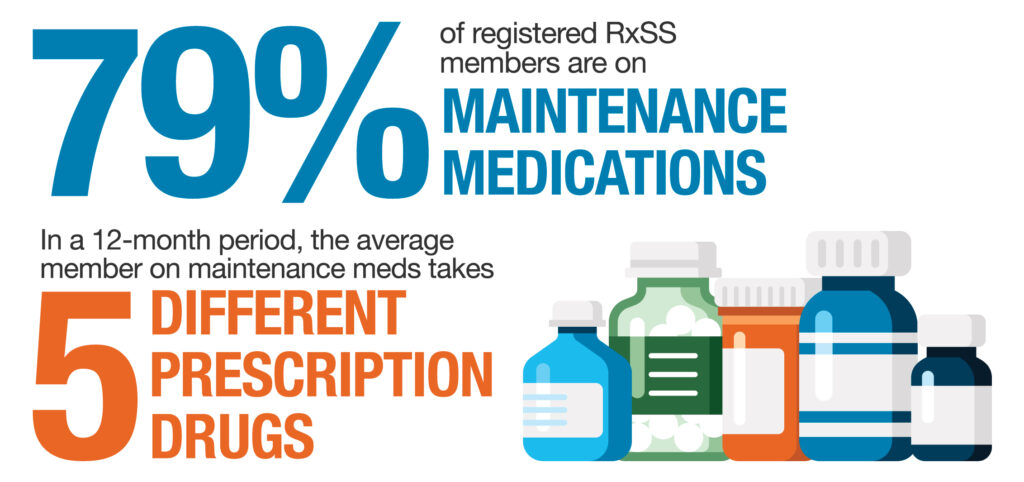
Every prescription tells a story, and Rx Savings Solutions analyzes millions of them. Most are written for common chronic conditions for members across every industry, job type, and in every region of the country. Nearly eight in 10 members who use us are on at least one maintenance medication. The average member of that group takes five different prescription drugs in a 12-month span, indicating many are battling multiple conditions or risk factors.
What happens when someone with diabetes does all the right things—engages with a diabetes point solution, follows a personalized management plan, never misses a telehealth appointment—but has to skip or ration their metformin, insulin or statin treatments? Poor health outcomes. Medication adherence is that important.
‘ANOTHER Point Solution?’
The strength of a point solution is also its weakness: It’s usually aimed at only one condition. Employers and health plans are seeing plenty of performance and potential in them, however, which explains why solution stacks continue to grow. We learned at HLTH ’21 that the average large, self-insured employer has 16 different health and wellness vendors.
Some plans may be reluctant to add more. Benefit administrators must decide whether a point solution can deliver on its promises of engagement, ease of use, ROI, and a happier, healthier workforce. In order to get maximum pull-through with any chronic disease solution, be sure the pharmacy benefit can support all of them.
Without medication that members can access and afford, what’s the point?
