A couple years ago, I joined a not-so-exclusive club, the roughly one in two American adults taking at least one prescription every day.
The monthly fill is about $100, all out of pocket until I meet my deductible. Thankfully it’s a manageable expense, but there were many months in my life when it wouldn’t have been.
Given where I work, I had to pick the doctor’s brain during a follow-up telehealth visit. I asked if something else might work for me but cost less. I may as well have asked my mechanic.
Of course, my doc mentioned other options within the same drug class. He just had no clue how their costs would compare. At the time, I happened to have one eye on his Zoom window and the other on savings suggestions displayed in my Rx Savings Solutions account. The one I pitched to him? “Sure, that’s a no-brainer,” he said.
Without Fault, But Ultimately Responsible
He approved the larger dose of the same medication in a splitable tablet, which cut my price in half. Afterward, I had the same thought every enlightened RxSS member probably has: If it’s a “no-brainer,” why didn’t he prescribe it in the first place?
A byzantine pharmacy system makes it tedious if not impossible for prescribers to know what any drug, dose or form they prescribe will cost me or anyone else.
How can they? Every patient is a walking permutation of all variables that factor into their out-of-pocket cost:
- Insurance type and plan design (there are tens of thousands out there)
- The drug’s negotiated plan price
- Formulary and tier
- Member copay/coinsurance
- Deductible status and out-of-pocket maximum
Very few doctors have all that in hand today. Even when they do, most still can’t accurately estimate out-of-pocket costs. A telling study published in JAMA Network Open found that only 21% could.
That’s right—the only people with legal authority to prescribe medication lack the ability to make decisions with a critical factor in mind: cost. That’s a major contributor to so much unnecessary pharmacy spend. It also means doctors can play a huge role in eliminating it. They’re not alone.
Transparency in All the Right Places
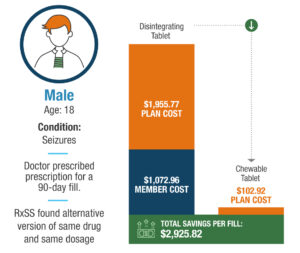
An actual example from Rx Savings Solutions member on anti-seizure medication: His doctor prescribed the oral-disintegrating form mistakenly believing it was cheaper than the chewable. [MORE on this story]
How could the unnecessary spend shown above have been avoided?
- If the patient had a digital resource for looking up out-of-pocket cost and available alternatives, either on demand or prompted by notification
- If the prescriber could quickly access the patient’s price and alternatives before prescribing
- If a care coordinator or someone else affiliated with the patient’s health plan could do the same at any point in the patient’s care journey
Routine RxSS claims analysis triggered a notification for the member above (actually sent to the member’s parent). They requested the lower-cost chewable tablet with one click. RxSS sent it to the prescribing physician. And like 85% of suggested switches RxSS sends to prescribers, it was quickly approved by the doctor.
Boom—the member’s family saved nearly $1,100 on one fill alone. The employer shaved off $1,800 from each successive fill.
Prescribers may write scripts with tunnel vision for therapies they’re familiar with and trust. We’re all creatures of habit. But when it comes to patient cost, most prescribe in total darkness.
No one can blame them, but we can empower them to write the most affordable prescriptions. Patients and their care teams should be equipped with the same transparency into costs and clinical alternatives.
When there’s transparency at all angles, light can be shed wherever it’s missing.

Did you know RxSS just launched a new Direct to Prescriber feature?
Learn how we’re closing a critical cost transparency gap.



